 Polycystic Ovary Syndrome, or PCOS, is a common hormonal disorder characterized by enlarged ovaries with multiple small cysts. It is a leading cause of high testosterone levels in women. PCOS disrupts the normal hormonal balance, resulting in excessive testosterone production.
Polycystic Ovary Syndrome, or PCOS, is a common hormonal disorder characterized by enlarged ovaries with multiple small cysts. It is a leading cause of high testosterone levels in women. PCOS disrupts the normal hormonal balance, resulting in excessive testosterone production.
What is Polycystic Ovary Syndrome (PCOS)?
PCOS is a medical condition that causes irregular menstrual periods, such as missed periods or overly long periods. In women with PCOS, small such-like cysts appear on the ovaries. The condition is also characterized by increased levels of male hormones (androgens) and the associated symptoms of high testosterone in women, such as excess body hair, acne, and male pattern baldness. The condition is fairly common, occurring in as much as 10% of adult women in the US.
The exact causes of PCOS remain unknown. While the condition is not 100% curable, it is treatable with a number of medical interventions and lifestyle changes that have been shown to reduce or minimize the most bothersome symptoms. In most women, once the condition is recognized and treated, patients with PCOS can go on to lead a normal life without significant complications. Although women with PCOS who want to become pregnant may need to take fertility medications to stimulate normal ovulation.
Causes and Symptoms of PCOS
The exact causes of PCOS are still not completely understood. However, it is intimately related to hormones, ovulation, and regular menstruation. While a woman is in her fertile or childbearing years, during monthly ovulation, a mature egg is released from an ovary and lies in wait in the uterus to be fertilized by a male sperm. If the egg is not fertilized, it is sent out of the body during a woman’s regular menstrual period.
However, when a woman is not ovulating normally due to a hormonal imbalance or other condition, multiple small cysts can form on the ovaries, and these cysts make and secrete testosterone, which leads to high testosterone in women and many of the symptoms of PCOS.
Many females with PCOS are overweight or obese, and they are at higher-than-average risk of developing type 2 diabetes, sleep apnea, fatty liver, and depression. These are all conditions that can lead to hormonal imbalances in women and, therefore, throw off normal ovulation and menstruation and also contribute to the development of PCOS.
Diagnosis and Treatment Options
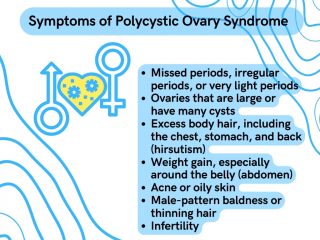
There are symptoms that you or your healthcare provider can look for that could indicate PCOS, such as:
However, in order to make an accurate diagnosis of PCOS, one or more tests will have to be done, such as an ultrasound of the ovaries to look for the cysts typical of the condition and or blood tests to check your testosterone levels. A woman’s body does make testosterone, and testosterone does play a role in the female body; however, in a woman with PCOS, her testosterone levels will be significantly higher than the small amount that is normal for a woman.
Impact on Hormones and Hormonal Imbalance in PCOS
As already mentioned, PCOS can cause a woman to produce excessive amounts of testosterone. This increased level of testosterone can cause many of the symptoms mentioned above, including infertility.
PCOS is also associated with elevated blood insulin levels. Insulin is a very important hormone to metabolism as it regulates the levels of glucose in the blood. Due to its impact on insulin, PCOS often leads to insulin resistance, obesity, and an increased risk of diabetes and non-alcoholic fatty liver disease in women with the condition.
Effects on Other Hormones
PCOS impacts other hormones besides insulin and testosterone. In females with PCOS, menstrual cycles are typically irregular, and normal ovulation does not occur; as a result, the levels of estrogen, progesterone, LH, and FSH all become imbalanced.
When ovulation does not occur normally, the ovaries do not produce progesterone, and the uterus’s lining becomes thicker and may shed irregularly. This is why heavy and/or prolonged bleeding is a common symptom of PCOS. Over time, this irregular growth of the uterine line can lead to endometrial overgrowth (called endometrial hyperplasia) or even endometrial cancer.
Role of Insulin Resistance in PCOS
Women with PCOS often are overweight and exhibit insulin resistance. Once a person is insulin resistant, glucose levels in the blood remain high as sugars do not travel into cells to be used for energy as they should. Insulin resistance often grows into glucose intolerance, a condition that is also referred to as “prediabetes,” which can ultimately lead to the development of type 2 diabetes.
Everyday Challenges of PCOS
Irregular menstrual cycles are not the only everyday challenge of living with PCOS; there are also the aforementioned issues with high testosterone, insulin resistance, and obesity, as well as fertility issues and impacts on emotional health and well-being.
Fertility Issues and Reproductive Health
Since women with PCOS are not ovulating regularly, it can take them longer to become pregnant, if they can conceive at all. Women with PCOS who desire to become pregnant should seek a fertility evaluation right away, as the chance of becoming pregnant with PCOS is quite low without fertility treatments.
Emotional Well-being and Mental Health
Women with PCOS tend to suffer from depression. This is likely due not only to the hormonal imbalances caused by PCOS but also the additional stress and self-esteem issues the condition can cause.
A 2021 study found that “women with PCOS have up to eight times higher prevalence of depression than control groups.” Other studies have found that women with PCOS are more likely than other females to experience problems with libido and sexual satisfaction and are more prone to suffer from eating disorders such as bulimia and binge eating.
How is PCOS Treated?
Treatments for PCOS are focused on minimizing your most troublesome symptoms and usually entail a combination of medication and lifestyle modifications.
Lifestyle Modifications
Since weight gain and obesity are a main cause of many of the problems related to PCOS, any weight loss can help. That means if weight gain or insulin resistance is one of your issues with PCOS, then diet and exercise will be a main part of your PCOS treatment plan.
Diet and Exercise for PCOS Management
Weight loss through a low-calorie diet combined with moderate exercise activities can make a significant difference in PCOS symptoms. Even moderate weight loss, like losing only about 5% of your total body weight, could significantly improve your PCOS symptoms. If you are also taking any medication to manage your symptoms, as you most likely will be, dropping a few pounds could increase the effectiveness of your medications and could also help with infertility. As to the best diet and exercise to manage your symptoms, that will be up to your doctor, your chief complaints, and your overall fitness level.
Exercise and Physical Activity Recommendations
Specific exercises recommended for you will depend on your most bothersome symptoms, how much weight your healthcare provider thinks you have to lose, and your overall fitness level. However, generally speaking, any increase in physical activity can help you lose weight, better manage your PCOS symptoms, and improve your overall health. That means you do not have to go out and join a gym — just get moving!
Park a little further from the store when you go shopping, try taking the stairs instead of the elevator, wash your car, swim, go bowling, or play tennis. Anything that ups your heart rate and strengthens your muscles can do wonders!
Stress Management Techniques
In addition to diet and physical activities, taking measures to reduce stress can help bring your hormones back into balance and reduce your PCOS symptoms. You may want to try engaging in some specific stress-reducing activities such as yoga, Tai Chi, or meditation – but if not, here are a few things you can do every day to help you calm down and combat daily stress.
- Practice acceptance – Many people get distressed over things they won’t let themselves accept. Often, these are things that can’t be changed. Try accepting the things you can’t change and stop stressing over them.
- Get a good night’s sleep – It is recommended that you get at least 8 hours of sleep.
- Get organized – Develop a realistic schedule of daily activities that includes time for work, sleep, relationships, and recreation.
- Reduce time urgency – Slow down, pace, not race; if you are the kind of person who frequently checks your watch, learn to take things a bit more slowly.
- Learn to delegate – You can’t be responsible all the time; stop trying to do everything yourself and start getting help from others.
- Talk to friends – Friendship is good medicine. Daily doses of conversation, regular social engagements, and occasional sharing of deep feelings and thoughts are excellent stress reducers.
Medical Interventions for PCOS
Medical interventions to relieve PCOS symptoms center around bringing hormones back into balance or specific medications to treat particular issues, such as fertility or returning regular periods.
Medications for Hormonal Regulation
To better regulate your hormonal balance and return normal periods, depending on your symptoms, your doctor may recommend combination birth control pills, which are designed to regulate both progesterone and estrogen levels and decrease testosterone. He or she may also recommend progesterone therapy only. But this kind of progestin therapy doesn’t improve androgen levels and won’t prevent pregnancy.
If you wish to become pregnant, your doctor may put you on medications that can improve fertility. If you are showing signs of prediabetes or diabetes due to PCOS, your doctor may put you on medications to control type 2 diabetes, some of the latest of which, such as Mounjaro and Ozempic, may also help you to lose weight.
Conclusions
PCOS is a fairly common hormonal condition in women, which, if left untreated, can cause day-to-day inconveniences as well as some serious health issues. While there is no technical cure for PCOS, it can be effectively managed, and its most serious symptoms reduced with lifestyle changes and proper medical interventions.

