The human immune system is the sum total of the body’s defense mechanisms against invading pathogens like bacteria and viruses. In a world full of such pathogens circulating in the air, food, and water, a well-functioning immune system is absolutely necessary for an organism to thrive. In fact, a lot can go wrong with an immune system, sometimes wreaking havoc on human health. In the 21st century, we are in the midst of a slow-burning autoimmune disease epidemic.
Autoimmune disease involves the mistaken identity by the immune system of healthy human tissue for an invading pathogen. The immune system springs into action, attacking the body’s own cells. Some autoimmune conditions are not serious, such as minor allergies, but others can be devastating. Multiple sclerosis, rheumatoid arthritis, and lupus are all autoimmune diseases.
In addition to autoimmune disease, malfunctioning immune systems have been implicated in a number of chronic health conditions. One of the primary roles of the immune system is, during times of attack by pathogens, to induce inflammation, the process of rushing white blood cells and other immune cells to the site of an attack or perceived attack.
In healthy people, inflammation is tightly regulated – the immune system dials inflammation levels up in times of crisis and down in times of normalcy. In unhealthy people, though, inflammation runs unchecked throughout the body. It is no exaggeration to say that inflammation fuels nearly all chronic disease. Although its HGH’s other roles in the body are more often highlighted, many people, even hormone replacement therapy patients, may not be aware of the complex and deep relationship between growth hormone levels and the immune system.
Here is a brief introduction to how the endocrine (hormone) system and immune system work together, as well as what tole HGH plays specifically in the process.
How Do the Immune and Neuroendocrine Systems Affect Each Other?
As a general rule, all the body’s systems are intertwined. What affects one affects the other. This rule of thumb is as true of the relationship between the immune and neuroendocrine systems as with all the rest.
“Neuroendocrine” refers to the coordinated activity of neurons (brain cells), glands, and non-endocrine tissues. Neuroendocrinology is the study of the relationship between the nervous system and hormone system, which are closely linked.
The immune system and neuroendocrine systems work together closely to maintain homeostasis and effectively combat pathogenic threats. The relationship between the two is bi-directional, meaning they both exert influences on each other. Hence, a well-functioning immune system helps support the neuroendocrine system’s activity and vice versa. The two systems are constantly “talking” to each other through cell signaling. To effectively kill invading pathogens without harming human cells while keeping inflammation in check, both systems must be running optimally.
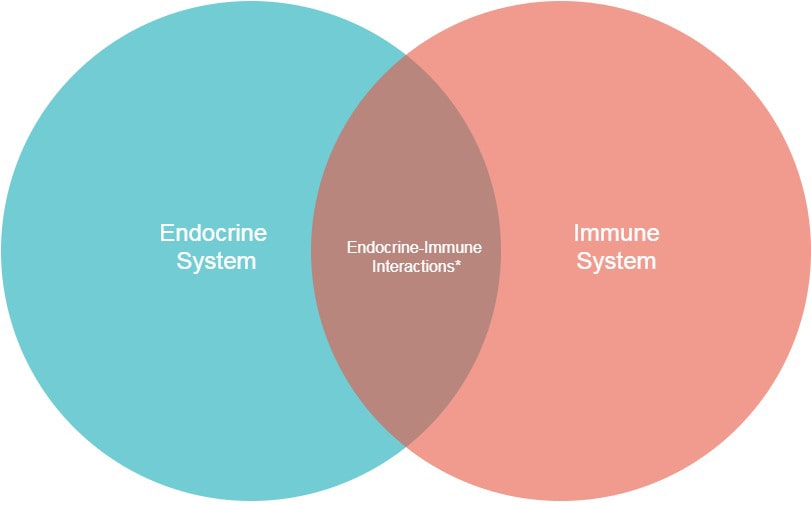
*Endocrine-Immune interactions (e.g. hormonal regulation of immunity, cytokine/ chemokine activation of endocrine cells)
Growth Hormone and Insulin-like Growth Factor-I (GH/IGF-I)
A major point of confusion for many when they are first introduced to growth hormone is the difference between HGH and insulin-like growth factor-1, or IGF-1.
The frequent mistaking of one for the other is understandable: they are both steroid hormones that work synergistically with one another. They both work to regulate the building of muscle, regulate body composition, and keep metabolism in check. Because GH stimulates the production of IGF-1 in the liver, their levels in the blood are correlated – higher HG means higher IGF-1. In the blood, their activity complements each other by mutual modification of effects.
There are, however, crucial distinctions between the two. First, growth hormone is produced in the brain in a small region called the pituitary gland, where many hormones are produced. IGF-1, on the other hand, is produced and released via the liver. Whereas HGH acts directly on targeted cells, IGF-1 exerts most of its influence indirectly.
How Does HGH Affect Immunoregulation?
Recent research explores HGH’s impressive immunoregulative activity. The conclusions of researchers are that HGH is involved in facilitating the following immunoregulatory activities in the body:
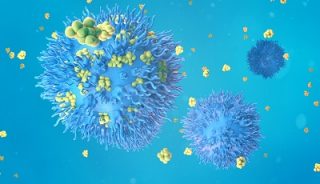
- HGH stimulates the production and release of T-cells (more on T-cells later)
- Aids in the development of myeloid progenitor cells. These cells serve as precursors to a variety of immune system cells, including macrophages, granulocytes, dendritic cells, and mast cells.
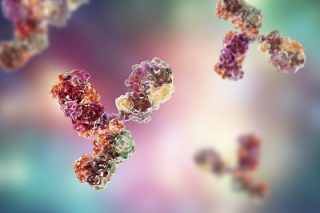
- Stimulates the synthesis of immunoglobulin. These molecules are produced by the immune system’s white blood cells. Their primary task is to attach themselves to antigens (viruses or bacteria) that the immune system is familiar with and kill them. Vaccines work by imitating particular viruses, prompting the immune system to produce immunoglobulin. In effect, this immunizes the patient from infection from that particular strain of virus or bacteria. Immunoglobulin molecules are often called “antibodies” for short. Through a complex signaling process, HGH enhances immunoglobulin production.
- Modulates cytokine response. Cytokines are crucial for overall immune system function. Specific immune system cells, predominantly macrophages, release these proteins that regulate homeostasis, coordinate immune responses throughout the body, and control inflammation. Out of control cytokine activity, sometimes called “cytokine storms”, can cause significant damage. HGH helps regulate its expression.
HGH’s Crucial Function for the Immune System
The increasing clinical evidence that HGH plays an integral role in the immune system’s activity has prompted new research into HGH’s role in HIV treatment. HGH stimulates growth of the thymus, the gland where the crucially important T-cells are produced and then released into the bloodstream. T-cells are the frontline defenders against invading pathogens. Specific types of T-cells called CD8+ cells are nicknamed “killer” cells because of their exceptional ability to eliminate both pathogens and human cells infected with those pathogens.
They patrol the body via the blood, neutralizing threats before they have time to spread to other areas or to proliferate. Without proper T-cell function or numbers, as is seen in advanced cases of HIV/AIDS, the body becomes exponentially more susceptible to infection. Viruses, bacteria, and fungi – normally easily defeated by the immune system – become
In addition to HIV/AIDS, many conditions can hamper the immune system’s ability to protect the body. HGH therapy holds promise, although more research is required, because of its stimulating activity on the immune system.
Options for Boosting HGH Levels
Now that we’ve established the value of HGH for a healthy immune system, in addition to its other benefits, how can you make sure that you have enough circulating HGH to meet your body’s needs?
The first step is to get tested. Most patients with low HGH have no idea about their hormone deficiency. Many have received unnecessary treatment for secondary symptoms related to growth hormone deficiency without addressing the root cause. Any reputable provider will begin a consultation with a quick and easy hormone test to measure your levels. If you do have a GH deficiency, then you have two options for treatment.
Natural Remedies

- The idea that people need three square meals a day, staying in a “fed” state all day, to stay healthy does not hold scientific weight. In fact, many studies on intermittent fasting now show the opposite – that, intermittent fasting supercharges your body’s processes, including the activity of the endocrine system. Intermittent fasting is the practice of reducing calorie intake to 0 for specific time periods each day, between 16-22 hours of no eating. After just 16 hours of fasting, levels of HGH are boosted. They stay elevated until the next feeding. The research into intermittent fasting is fascinating, and the evidence continues to roll in that this lifestyle adjustment holds massive healing power.

- Losing weight through a healthy diet and exercise can boost HGH levels. Growth hormone levels are negatively correlated to body fat percentages, meaning that the more fat you have, the lower amounts of GH are released by the pituitary gland.

- Sleep is absolutely the best thing that most people can do for struggling endocrine systems. During times of slumber is when the repair work for the body switches into high gear, replacing old cells, restocking hormone levels, and boosting immune function.
Replacement Therapy
For some patients, making lifestyle adjustments is not sufficient to restore Growth Hormone to optimal levels. In these instances, Hormone Replacement Therapy (HRT) might be the next treatment plan.

The process of GH replacement therapy is straightforward: your GH levels are measured during blood work, the dose is calibrated to make up the deficit, a simple injection is made, and regular follow-up visits will confirm the effectiveness of the treatment through further blood tests as the course of therapy moves on.
For many patients whose lives have been transformed with GH replacement therapy, this kind of work has been a godsend. They have rediscovered their lust for life, they have more energy, and they feel younger than ever before – all thanks to a simple hormone.
If you are considering treatment, give HGH Therapy Clinic a call today. We’re always available to set up a no-hassle consultation appointment with an experienced therapy provider to discuss your treatment options.