Hysterectomy is a common medical procedure in the United States. People may also be familiar with hysterectomy as “surgical menopause”. About 600,000 American women receive hysterectomies each year. As we will explore in this article, hysterectomy comes with accompanying side effects. Much of the body changes following hysterectomy occur in the endocrine system, the body’s delicate hormonal system that plays a vital role in health.
Here you’ll find a brief introduction to hysterectomy, the different types of hysterectomy, its effects on hormone levels, and what patients can do to correct imbalances caused by the procedure.
Typical Hormone Levels in Healthy People
Hormone levels naturally fluctuate throughout life. In both males and females, the relative level of both estrogen and testosterone rise during puberty, peak during reproductive prime, and steadily decrease afterward.
What is Hysterectomy and Oophorectomy?
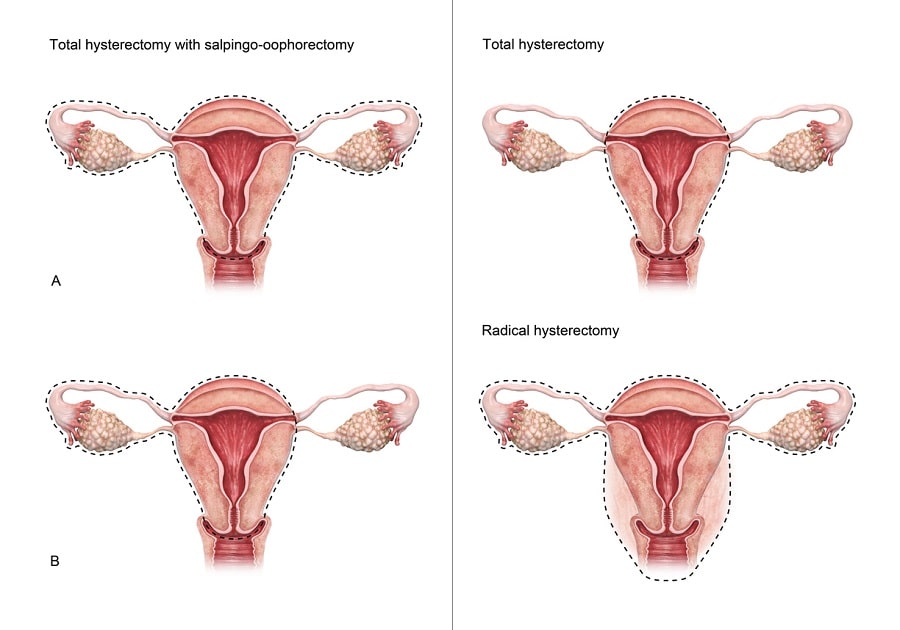
“Hysterectomy” is the medical term for the removal of a woman’s uterus. Sometimes, the ovaries, cervix, and other parts of the reproductive system must be removed as well. When the ovaries are removed, that is called an “oophorectomy”. Both procedures are usually performed by a gynecologist, a doctor who specializes in women’s reproductive medicine.
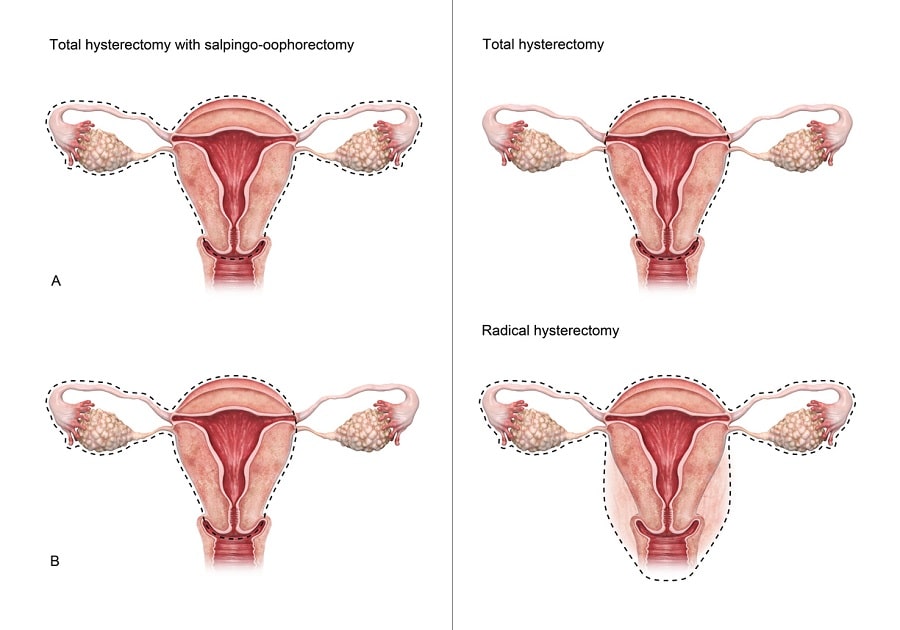
Full vs. Partial Hysterectomy
Hysterectomy procedures are divided into two categories: “full” hysterectomy (also known as “total” hysterectomy) and “partial” hysterectomy. A partial hysterectomy involves the removal of the uterus alone while the cervix remains intact. Full hysterectomy means the removal of the cervix in addition to the uterus. The procedure can also involve the removal of the fallopian tubes and the ovaries.
The reasons for a hysterectomy / oophorectomy vary. The most common situations that necessitate the removal of the uterus are cancer, pelvic pain, heavy menstruation, and a condition called endometriosis in which tissue that should normally grow inside the uterus instead grows outside of it. Women who get hysterectomies are no longer able to bear children. There is some risk of injury or even death during surgery, though such events are rare.
 Because the reproductive system is altered during a hysterectomy, the procedure has a significant impact on hormones – specifically, the so-called “sex hormones” testosterone, estrogen, and progesterone. Maintaining the right levels of each, in proper ratios to one another, is crucial for health.
Because the reproductive system is altered during a hysterectomy, the procedure has a significant impact on hormones – specifically, the so-called “sex hormones” testosterone, estrogen, and progesterone. Maintaining the right levels of each, in proper ratios to one another, is crucial for health.
Many women who have undergone hysterectomy report side effects that are often caused by these hormonal changes. Examples include:
- Insomnia
- Irritability
- Vaginal dryness
- Painful intercourse
Hysterectomy is a common procedure that triggers significant changes to the hormonal system.
How Does a Hysterectomy Affect Hormone Levels?
Hysterectomies typically have large and noticeable effects on hormone levels as measured through blood samples. The problem of substantially reduced estrogen caused by removal of the uterus and/or ovaries has been well documented, and so far there is no known method for removing the uterus and/or ovaries without causing these complications.
The changes following hysterectomy for the endocrine system are usually significant.
Before Hysterectomy
Almost all of the estrogen that women produce until their 50s is sourced from the ovaries. Estrogen is the chief female sex hormone, and its stable presence in the blood is important. According to most doctors, estrogen levels in menstruating women hover between 15 to 350 picograms per milliliter (pg/mL). Women who have undergone menopause, whether natural or surgical, typically have less than 10 pg/mL.
After Hysterectomy
Following removal of the uterus and/or ovaries, levels drop substantially. Estrogen and progesterone levels, the two primary female sex hormones, drop naturally and considerably throughout life. To help better understand how these hormone levels change over the course of a woman’s life, here is a chart illustrating a typical change:
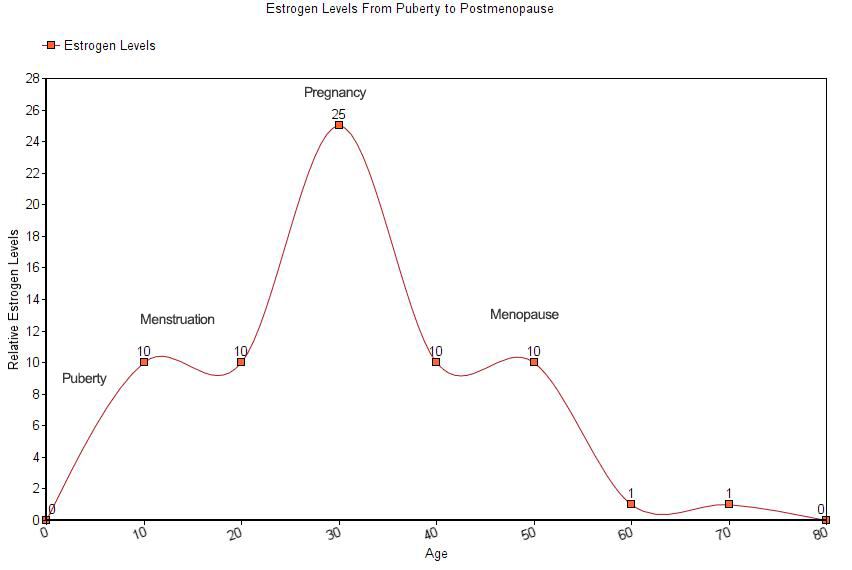
For women who receive hysterectomies, even young women, the downward trajectory of estrogen is similar to a woman who has undergone natural menopause. For these women, replacing hormones through therapeutic administration can help restore estrogen and progesterone levels to more ideal levels.
Hormone Replacement for Restoring Hormones to Healthy Levels
Hormone Replacement Therapy (HRT) is the practice of replacing natural hormone levels with synthetic hormones through oral medications, through patches or gels that supply estrogen which is absorbed through the skin, or through an injection or a series of injections. The provider will first measure the patient’s blood serum levels of the hormone in question, then titrate the right dosage to achieve optimal levels. Throughout the course of treatment, the doctor will closely monitor hormone levels as well as vital signs to make sure no adverse reactions occur. Once the right concentration in the blood is measured, the therapy is complete. Many people, however, must come back at regular intervals for additional doses of the hormone or hormones that they need.
Estrogen therapy (ET) is a type of HRT that replaces estrogen levels – critical for female patients who want to recover the quality of life they enjoyed before hysterectomy. The therapy involves the administration of the two primary female sex hormones, progesterone and estrogen.
ET can include either estrogen alone or estrogen and progesterone together. Studies have proven estrogen to be the most effective known treatment for treating postmenopausal symptoms, both surgical and natural.
Choosing the right provider who will take the necessary precautions and monitor the patient’s health throughout therapy is crucial to get the best results with the least side effects.
Most patients respond well to treatment and experience no complications.
How to Optimize Hormone Replacement Therapy
 For many women, time is of the essence when it comes to getting necessary hormone replacement therapy. In one study of young women with a medical condition that required hysterectomy and who had later received HRT, the researchers found that women in the control group who had not received replacement therapy following their hysterectomies were substantially more likely to develop osteoporosis than their counterparts who had received the replacement therapy. Likewise, the risk of specific types of cancer increases with untreated hormonal changes like those experienced following surgical menopause. Therefore, it’s imperative that women who might benefit from HRT act quickly to reap the biggest benefit.
For many women, time is of the essence when it comes to getting necessary hormone replacement therapy. In one study of young women with a medical condition that required hysterectomy and who had later received HRT, the researchers found that women in the control group who had not received replacement therapy following their hysterectomies were substantially more likely to develop osteoporosis than their counterparts who had received the replacement therapy. Likewise, the risk of specific types of cancer increases with untreated hormonal changes like those experienced following surgical menopause. Therefore, it’s imperative that women who might benefit from HRT act quickly to reap the biggest benefit.
Studies have also demonstrated the importance of individualized ET treatment for the most successful outcome. High-performing doctors, therefore, meet with patients beforehand, evaluate them, discuss options, and develops a personalized treatment plan based on the patient’s needs and desires.
Never settle for a doctor who seems disinterested in your particular case. Instead, seek one out that displays a genuine interest in getting the best health outcome for you and who takes the time to discuss your situation.
The Takeaway
Women may require a hysterectomy for a variety of reasons. Once important parts of the female reproductive system are removed, hormone levels in the blood are altered significantly. Estrogen therapy can help restore estrogen and progesterone, the most important female sex hormones, to their optimal levels following surgical menopause. Many women find massive relief from postmenopausal symptoms and a restored quality of life following hormone replacement therapy.