Hormone Replacement Therapy and Hysterectomy
 Women who go through natural menopause experience a slow decline in hormone production. The symptoms of menopause, if they occur at all, may also happen slowly. That is not the case for women who undergo a hysterectomy and oophorectomy. Surgical menopause often starts quickly, bringing with it a host of menopausal symptoms. That is the basis for this report on hormone replacement therapy and hysterectomy.
Women who go through natural menopause experience a slow decline in hormone production. The symptoms of menopause, if they occur at all, may also happen slowly. That is not the case for women who undergo a hysterectomy and oophorectomy. Surgical menopause often starts quickly, bringing with it a host of menopausal symptoms. That is the basis for this report on hormone replacement therapy and hysterectomy.
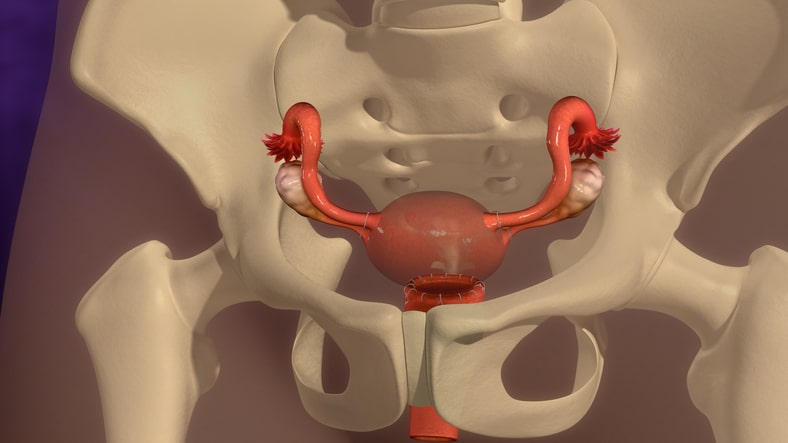
Now, just because a woman undergoes a hysterectomy does not mean she will enter menopause. If the doctor leaves behind the ovaries, she will continue to produce the hormones progesterone, testosterone, and estrogen. It is only when an oophorectomy removes the ovaries will a female experiences a decline in hormone levels.
There are also differences between the types of hormone replacement therapy for hysterectomy following surgery. The treatment depends on whether ovarian removal occurred, or if just the uterus was removed.
There is also a difference in the use of hormone replacement therapy without hysterectomy. The doctor will determine the type of treatment best suited to each woman’s needs.
Hormone replacement therapy after a hysterectomy depends on symptoms, and whether the ovaries were removed.
What Is Surgical Menopause and How Does Hormone Therapy Help?
Surgical menopause applies to the situation that develops when a woman has her ovaries removed in an oophorectomy. As soon as the ovaries leave the body, hormone production drops exponentially. Although other parts of the body continue to produce estrogen, testosterone, and progesterone in small amounts, it is not enough to make up the difference of what the ovaries provided. That is why hormone replacement therapy after hysterectomy is so important.
For many women, the signs of menopause, such as night sweats, hot flashes, weight gain, brain fog, and depression can come on fast and furious. Doctors typically do not remove both ovaries without also taking the uterus due to endometrial cancer risk. However, uterine removal without taking the ovaries is possible. A woman who still has her ovaries will not enter surgical menopause.
When discussing hormone replacement therapy and hysterectomy, it is often recommended to use estrogen therapy for at least a short time after an oophorectomy. The immediate decline in hormone levels can lead to:
- Vaginal dryness
- Low libido
- Loss of bone density
- Night sweats
- Hot flashes
- Depression
- Weight gain
- Memory loss
Younger women under 45 who undergo an oophorectomy increase their risk of developing neurological and heart diseases, as well as cancer if they do not receive hormone replacement therapy. Surgical menopause after ovarian removal (oophorectomy) which causes an immediate decline in hormone levels.
What Type of Hormone Therapy Do You Need After a Hysterectomy?
 Although it may not always be needed, HRT is often recommended – at least for a short time – following an oophorectomy. The immediate drop in hormone production may not cause hot flashes and mood swings, but it may impact one’s bones, heart, or brain functions.
Although it may not always be needed, HRT is often recommended – at least for a short time – following an oophorectomy. The immediate drop in hormone production may not cause hot flashes and mood swings, but it may impact one’s bones, heart, or brain functions.
In the following hormone replacement therapy guidelines, hysterectomy and oophorectomy needs are explained:
- Hormone therapy options following an oophorectomy and hysterectomy:
- Estrogen therapy
- Progesterone therapy – women without their ovaries should not use synthetic progestin as that can increase certain side effect risks – only natural or bioidentical progesterone therapy is advised
- Hormone replacement options following only a hysterectomy with the ovaries still intact:
- Estrogen therapy
- Progesterone (bioidentical)
- Progestin – synthetic (still not the best choice)
- Hormone therapy after an oophorectomy with the uterus still in place:
- Estrogen and progesterone therapy combined – crucial to protect against endometrial cancer
While those are the standard guidelines for hormone replacement, there are other options that every woman should know:
- Human growth hormone (HGH) therapy – many menopausal women are also deficient in growth hormone which has similar symptoms to menopause. HGH therapy often reverses the symptoms of menopause in women. It will help strengthen bones, sharpen brain functions, stimulate fat burning, and reduce hot flashes and night sweats. HGH also improves vaginal secretions and libido.
- Testosterone replacement therapy (TRT) – testosterone is the natural precursor hormone to estrogen, making it essential for a woman’s body. Testosterone is also safe for many women who cannot take estrogen.
- Calcium and vitamin D – these are advisable to protect bones from becoming weak.
- Black cohosh – often helps reduce hot flashes for women.
Understanding hormone replacement therapy and hysterectomy needs are crucial so that you ensure you are getting the right treatment.
Women who have their uterus intact and only undergo ovarian removal need progesterone to reduce the risk of endometrial cancer.
Does an Oophorectomy Change the Type of Hormone Therapy You Need?
Determining the proper type of hormone replacement therapy after hysterectomy is crucial for safety and efficacy. The most important aspect that we mentioned in the last section is for women who undergo only an oophorectomy. If a woman still has her uterus, she must receive supplemental progesterone to protect against endometrial cancer.
When considering the facts about hormone replacement therapy and hysterectomy, you also want to keep in mind the following:
- Take the lowest effective dosage possible
- Use hormone replacement therapy for the shortest time
- Turn to bioidentical rather than synthetic hormones whenever possible
- Speak with a hormone specialist to discuss options, not just a gynecologist or primary care physician
Seek the guidance of a hormone specialist when discussing options for hormone replacement therapy.
Are There Side Effects of Hormone Therapy after a Hysterectomy?
 No medical treatment is without risks. Women are naturally concerned over side effects of hormone therapy following earlier studies that shed light on heart attack and breast cancer risks. That is why we strongly recommend working with a hormone specialist who has extensive training in this field.
No medical treatment is without risks. Women are naturally concerned over side effects of hormone therapy following earlier studies that shed light on heart attack and breast cancer risks. That is why we strongly recommend working with a hormone specialist who has extensive training in this field.
The most common hormone replacement therapy after hysterectomy side effects include:
- Headaches
- Weight gain
- Swollen breasts
- Nausea
- Breast pain
Then there are also the increased risks of developing:
- Breast cancer
- Blood clots
- Stroke
- Heart attack
- Gallstones
- Ovarian cancer
Ultimately, the choice is up to each woman. If you are over the age of 50 when you have an oophorectomy and hysterectomy, you may want to leave it to nature, as this is the time your body would likely enter menopause. Of course, if symptoms are severe or there is a concern of osteoporosis, HRT is highly recommended.
To learn more about bioidentical hormone replacement therapy and hysterectomy, please contact our hormone clinic for a free consultation.
Side effects and risk factors for bioidentical hormone therapy are slight. Contact our hormone clinic for more information during a confidential, free consultation.

