Protecting bone health is a critical part of any anti-aging strategy. Over time, as we age, the bones tend to lose density and, as a result, become more prone to fractures due to falls or other accidents. Here, we will discuss the most important aspects of bone health, how aging affects the bones, and methods you can use (including HGH replacement therapy) to mitigate bone loss across time with the goal of keeping the bones strong and healthy late into life.
Bone Health and Diseases That Affect the Bones
As the human body ages, the risk of developing certain conditions and diseases affecting the bones increases. For this reason, anti-aging science has focused heavily on strategies to mitigate this risk and ensure that bones stay healthy and strong late into life.
How Bones Form and Develop
 Bone development, in scientific terms, is referred to as osteogenesis or ossification. Let’s explore the step-by-step process of bone development from the beginning. In the initial stages of development (the fetal stage), a baby’s bones grow in two phases:
Bone development, in scientific terms, is referred to as osteogenesis or ossification. Let’s explore the step-by-step process of bone development from the beginning. In the initial stages of development (the fetal stage), a baby’s bones grow in two phases:
- Intramembranous ossification. At this stage, “spongy” bone develops to form the flat bones of the face, the cranial bones, and the clavicle (collarbone).
- Endochondral ossification. Here, specialized cells called chondrocytes divide to form bone tissue in place of cartilage to begin to form the skeleton. At this point, the bones begin to thicken as well as lengthen – a process called appositional growth.
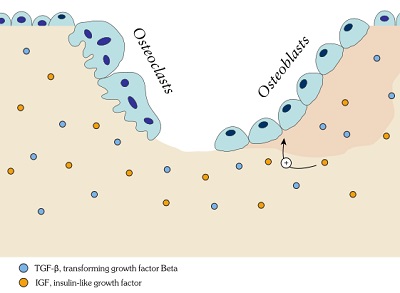
Following birth, humans then enter the next phase of bone development called secondary ossification. During this period, a structure on the ends of the bones called the epiphysis where the bones continue to lengthen and thicken throughout childhood and adolescence. In the third stage of bone development – which continues throughout life – the bones go through remodeling. During bone remodeling, specialized cells called osteoclasts and osteoblasts remove bone material and lay down new material, respectively.
This process of continual bone remodeling into adulthood is mediated by a combination of cells called cytokines, as well as hormones, that include:
- Transforming growth factor-beta (TGF-β)
- Insulin-like growth factor 1 (IGF-1)
- Parathyroid hormone (PTH)
- Calcitriol
- Sex hormones (primarily testosterone in men and estrogen in women)
- Glucocorticoids (steroid hormones that support healthy bone remodeling)
- Human growth hormone (HGH)
Aging, Bone Health, and the Risk of Osteoporotic Fractures
 Bones thicken through the processes described in the previous section during the early phases of life. Bone density, as seen in the chart below, tends to peak around age 30. Thick bones do not break as easily and support greater muscle mass.
Bones thicken through the processes described in the previous section during the early phases of life. Bone density, as seen in the chart below, tends to peak around age 30. Thick bones do not break as easily and support greater muscle mass.
Therefore, preserving bone density is critical for preventing fractures commonly experienced by older adults. Over time, following the peak in bone density around age 30, the human body tends to lose bone density steadily.
However, it’s important to note that age-related loss of bone density is by no means inevitable. There is no law written in stone that mandates bone density loss. The current state of anti-aging science is highly advanced, and medical science knows much more now than even a decade ago in terms of how to slow, prevent, and even reverse losses in bone density in aging patients.
Nutrition and Lifestyle Practices Essential For Healthy Bones
If you are concerned about bone density (as anyone over the age of 40 should be), then you have several tools at your disposal to prevent the process of progressive bone loss. Here are the key bone-fortifying strategies: based on the science:
- Eat a balanced, whole foods-based diet. Opt for plenty of fresh vegetables, healthy (unprocessed) lean meats, calcium-rich and other whole foods. Eliminate or limit processed “junk” foods such as snack bars, candies, sodas, chips, crackers, etc.
- Calcium supplementation (when necessary). Calcium is important for keeping bones strong. Lab tests can confirm your calcium levels.
- Vitamin D supplementation (when necessary). Vitamin D, the “sunshine vitamin,” is another nutrient (that is technically a hormone) that is necessary for maintaining bone density. Unfortunately, an estimated 40% of the US adult population is deficient in this critical vitamin. Sunlight is an excellent source of vitamin D, along with certain foods such as shellfish and fortified dairy. Vitamin D supplements can also effectively raise blood concentrations.
- Regular exercise. Any type of exercise is beneficial for boosting the underlying physiological processes that support healthy bone remodeling, but none is better than high-intensity heavy lifting.
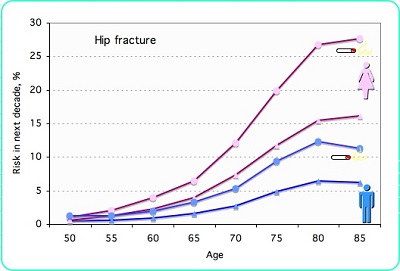
- Quit smoking and limit alcohol intake. Smoking, in particular, is devastating for bone health in a number of ways, including through exposure to the numerous toxic chemicals in cigarette smoke. The chart below demonstrates the substantially increased risk of smokers vs. non-smokers for hip fractures.
- Know your personal risk factors. Women have a greater risk of developing clinically significant bone loss (osteoporosis) compared to men. Likewise, whites and Asians have a greater risk compared to other races. Your family history of the disease is also important to weigh. An experienced endocrinologist (hormone doctor) or another anti-aging specialist can help determine your personal risk for developing bone disease and develop an individual protocol to protect your bone health accordingly.
Factors That Lead to Low Bone Density
The top factors that lead to low bone density include:
- Genetic predisposition
- Lack of proper exercise and activity levels
- Smoking and excessive alcohol use
- Inadequate calcium intake
- Chronic use of certain medications such as selective serotonin reuptake inhibitors (SSRIs), prednisone, aromatase inhibitors, dexamethasone methotrexate, anti-seizure medications, proton pump inhibitors, etc. Talk to your doctor about the medications you currently take to determine if they may have a negative impact on your bone health.
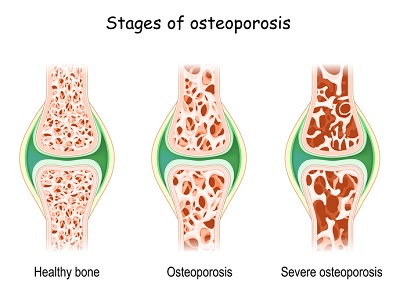
What Is Osteoporosis?
Osteoporosis refers to a chronic, age-related condition in which imbalances to the natural bone remodeling process cause resorption of bone material without proper replacement with new bone material. Over time, this leads to brittle, fragile bones that are more prone to fractures. Osteoporosis is often described in medical literature as a major public health threat. The condition is estimated by the International Osteoporosis Foundation (IOF), the leading global medical authority on the topic, to affect over 10 million American seniors. An additional 40 million are at high risk of developing osteoporosis. Over 80% of individuals affected by osteoporosis are women. The chart below details osteoporosis risk by sex and age.
Causes of Osteoporosis
 Oftentimes, pinpointing a single cause of osteoporosis is difficult. The vast majority of osteoporosis patients have multiple risk factors that combine to trigger the onset of the condition. These include:
Oftentimes, pinpointing a single cause of osteoporosis is difficult. The vast majority of osteoporosis patients have multiple risk factors that combine to trigger the onset of the condition. These include:
- Lack of adequate nutrition
- Family history
- Excessive drinking/smoking
- Lack of exercise
- Gastrointestinal disorders (poor gut health)
- Long-term use of certain medications
- Untreated rheumatoid arthritis
Hormonal imbalances and dysfunctions can also play a major role in triggering osteoporosis, such as:
- Overactive thyroid gland
- Sex hormone deficiencies (testosterone and estrogen)
- Overactive parathyroid glands
- Adrenal gland disorders like Cushing’s syndrome
- Human growth hormone (HGH) deficiency
Symptoms of Osteoporosis
The symptoms that indicate the presence of osteoporosis include:
- Chronic Back pain due to the fractured or damaged vertebra
- Progressive loss of height across age
Poor posture, most commonly in the form of stooping
- Abnormal fractures occurring when they should not
How Doctors Diagnose Osteoporosis
While the above symptoms might hint at osteoporosis, clinical testing is the only surefire method to diagnose the condition.
To diagnose osteoporosis, doctors typically perform a bone mineral density (BMD) scan. The two most common and reliable tests that definitively determine the presence of osteoporosis are:
- Dual-energy x-ray absorptiometry (DXA or DEXA)
- Bone densitometry
Other diagnostic tools that doctors often use to assess the presence or risk of osteoporosis include:
- CT scan of the spine
- MRI of the spine
- Bone x-ray
Conventional Treatments for Osteoporosis

The US Food and Drug Administration (FDA) has approved many medications specifically intended to treat osteoporosis. These include:
- RANK ligand inhibitor
- Selective estrogen receptor modulators (SERMs)
- Bisphosphonates
- Calcitonin
- Parathyroid hormone analog
- Hormone replacement therapy (HRT) – more on HRT later
In the case of compression fractures in the vertebra (spine) that occur due to osteoporosis, two types of corrective surgery may be employed:
- Vertebroplasty. In this procedure, surgeons inject a material called bone cement – medically known as polymethylmethacrylate (PMMA) — into the injured vertebra, which then hardens and, if successful, prevents further damage.
- Kyphoplasty. This procedure is similar to vertebroplasty, except that, in the case of kyphoplasty, surgeons use a small balloon to create a cavity, or open space, before injecting the bone cement.
HGH and Osteoporosis FAQs
 Let’s get into the complex and extremely important relationship between human growth hormone (HGH) and bone health. HGH is an anabolic hormone, which means that it promotes healthy growth and development of organs, glands, tissues, and bones. Its many activities in the body include:
Let’s get into the complex and extremely important relationship between human growth hormone (HGH) and bone health. HGH is an anabolic hormone, which means that it promotes healthy growth and development of organs, glands, tissues, and bones. Its many activities in the body include:
- Metabolism regulation (managing energy levels and burning fat)
- Protecting the heart and cardiovascular function
- Protein synthesis (muscle-building)
- Regulating mood and cognitive function
- Fortifying bone density
In a large segment of the population, especially seniors, HGH levels fall below the healthy thresholds in the chart below.
| Healthy HGH Levels | ||
| Adult Men | Adult Women | Children |
| 0.4-10 ng/mL | 1-14 ng/mL | 10 to 50 ng/mL |
When blood tests show abnormally low, unhealthy HGH levels per the above levels deemed to be healthy, the patient is diagnosed with growth hormone deficiency (GHD). The good news is that HGH replacement therapy with bioidentical HGH – a special type of HRT called bioidentical hormone replacement therapy (BHRT) – can effectively stop and reverse HGH deficiency by restoring healthy HGH levels.
- Does HGH Help to Treat Osteoporosis? Studies bear out the healing potential of HGH in cases of age-related loss of bone density: “For years after it was administered, growth hormone continued to reduce the risk of fractures and helped maintain bone density in postmenopausal women who had osteoporosis.”
- Can HGH Make Your Bones Grow? The answer depends on the type of growth in question. In adults, HGH will not spur bone lengthening, so it does not result in greater height. However, it does enhance the process of bone remodeling, in which the bones replenish and rethicken continually.
- Does HGH Increase Bone Density? In patients with GHD. HGH increases bone density and prevents fractures: “The rate of fractures in the treated women who had osteoporosis declined by 50 percent during the 10-year-long study. More than half of the participants had fractured bones prior to the start of the study. In contrast, the rate of fractures rose four-fold in the control group as some of those women were diagnosed with osteoporosis.”
What Role Does HGH Play in Optimizing Bone Health?
As we mentioned previously, HGH – in combination with its partner hormone, insulin-like growth factor 1 (IGF-1), and other hormones – is critically involved in regulating bone development and remodeling throughout the life cycle.
“Bone and mineral metabolism is regulated by numerous hormones and local growth factors. Growth hormone (GH), directly and/or indirectly through local IGF1 and IGF2 production, stimulates bone turnover as it increases osteoblast number and function. It also stimulates bone resorption through unknown mechanisms.”
Other Common Bone Conditions and Injuries in Aging Bodies
 Osteoporosis is not the only bone-related health concern for aging men and women. Other conditions that most often affect older individuals include:
Osteoporosis is not the only bone-related health concern for aging men and women. Other conditions that most often affect older individuals include:
- Osteopenia. This is a milder form of osteoporosis. Individuals with osteopenia are more likely than the average population to fracture a bone but less likely than someone with osteoporosis.
- Hip fracture. Hip fractures are the most concerning type of break in the elderly because the clinical data shows that “one in three adults aged 50 and over dies within 12 months of suffering a hip fracture.”
- Vertebral injuries and diseases. Also known as spinal cord injury (SCI) when they affect the nerves, SCIs are particularly damaging to the quality of life in the elderly and are associated with greater mortality. Proper preventative measures – including, when appropriate, HGH replacement therapy – should be employed as part of anti-aging care to prevent SCIs in seniors.
- Metabolic bone disease. This broad category of bone disease includes conditions associated with aging like rickets, Paget disease (often treated with Alendronate), osteomalacia, osteogenesis imperfecta, and fibrous dysplasia.
How to Prevent Osteoporosis and Other Bone Disease
Based on everything we have discussed so far, let’s get into the proven ways that men and women over 40 can reduce their risk of osteoporosis and other age-related bone conditions:
- Healthy diet. This means focusing on whole, unprocessed, ideally organic foods (especially ones high in calcium like while eliminating processed ones high in added sugar and preservatives.
- Calcium, vitamin D, and other supplements. Sometimes, getting enough nutrition via diet in terms of bone-protecting vitamins and nutrients is difficult. In these cases, your doctor may recommend one or more supplements to make up the difference.
- Regular Exercise. Exercise, next to a healthy diet, is the single most powerful natural medicine for increasing bone density. Exercise, particularly with weights, balances hormones and boosts the process of bone remodeling which, as we discussed previously, is critical for thickening the bones.
- Hormone replacement therapy (when appropriate). The clinical evidence showcased earlier is clear: for patients with a hormone deficiency that negatively impacts bone density, replacement therapy with bioidentical hormones (including HGH) replenishes bone density and keeps them strong.

