According to the CDC and other leading public health groups, only 12% of Americans have good metabolic health. 33% of Americans, on the other hand, demonstrate the clinical markers of sub-optimal metabolic function, a condition called metabolic syndrome. Poor metabolic health doesn’t affect overweight individuals only. Researchers from the University of North Carolina noted that metabolic function is often impaired even among people with normal weight.
Untreated metabolic syndrome results in a severe, negative impact on the quality of life of affected individuals. Over time, the condition significantly increases the likelihood of developing chronic, fatal conditions like heart disease and diabetes. With the right strategy, though, prevention of metabolic syndrome is possible. Metabolic health can also be recovered following the onset of metabolic syndrome under many circumstances.
In this article, you’ll find everything you need to know about metabolic syndrome, its causes and symptoms, and how the condition can be prevented and even reversed.
What Is Metabolic Syndrome?
 Metabolic syndrome essentially means that your body does not process, utilize, and store energy properly. Rather than being a single condition itself, metabolic syndrome is actually a combination (or “cluster”) of five conditions in one:
Metabolic syndrome essentially means that your body does not process, utilize, and store energy properly. Rather than being a single condition itself, metabolic syndrome is actually a combination (or “cluster”) of five conditions in one:
- Clinical obesity (BMI of 30 or above).
- High fasting blood sugar (as seen in diabetic patients).
- Elevated triglycerides.
- High blood pressure.
- Low levels of high-density lipoprotein (HDL) – healthy cholesterol.
If you have at least three of the above conditions (as assessed through a physical examination and lab work), then you qualify as having metabolic syndrome.
What Causes Metabolic Syndrome?
Researchers have invested a great share of resources in recent years into understanding the root causes of the troubling increase in metabolic syndrome rates. The causes of metabolic syndrome are many. They can include: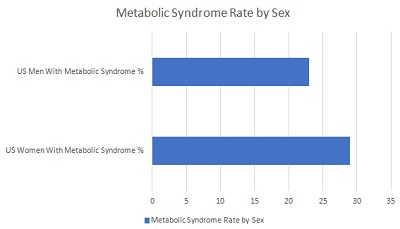
- Smoking. Cigarettes smokers experience higher rates of metabolic syndrome than non-smokers.
- Age. Rates of metabolic syndrome go up across the lifespan, with elderly Americans experiencing the highest incidence.
- Obesity. Higher fat accumulation impairs metabolic function.
- Diabetes. Individuals with diabetes also experience impaired metabolic function more frequently than non-diabetics.
- Sleep apnea. In addition to causing metabolic syndrome, sleep apnea and metabolic dysfunction in combination substantially increase the risk of heart disease.
As you will see below, the causes of metabolic syndromes can also be the symptoms of the disorder. For example, obesity can trigger the onset of metabolic disorder, which in turn can cause even more adipose tissue (body fat). This results in a vicious cycle of spiraling metabolic health and, ultimately, death if the pattern is not reversed.
What Are the Signs and Symptoms of Metabolic Syndrome?
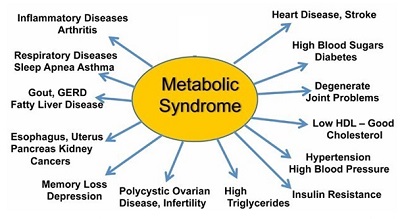
The symptoms of metabolic syndrome are widespread, affecting multiple organs and body functions. The symptoms of the disorder generally include:
- Loss of interest in sex (low libido).
- Joint pain.
- Unwanted weight gain (especially belly fat, also called “visceral fat”).
- Depression.
- Chronic fatigue (low energy).
- Fatty liver.
- High blood pressure.
In addition to triggering the symptoms above, metabolic syndrome also puts you at a higher risk of developing the following serious conditions:
- Heart disease.
- High LDL cholesterol (the harmful type).
- Low HDL cholesterol (the beneficial type).
- Arthritis and other autoimmune conditions.
- Stroke.
- Neurodegenerative diseases such as dementia, Alzheimer’s disease, and Parkinson’s disease.
Who Is at Greatest Risk of Developing Metabolic Syndrome?
There are several important risk factors to consider when evaluating the chances of developing metabolic syndrome on a case-by-case basis.
Individual and Lifestyle Risk Factors for Metabolic Syndrome
Lifestyle and individual health markers inform your personal risk of metabolic syndrome. The most important markers of your personal risk for developing metabolic syndrome are:
- BMI (obesity). A BMI of 25 or above puts you at risk of metabolic syndrome.
- Genetics. The International Federation of Clinical Chemistry and Laboratory Medicine notes that “a family history that includes obesity, type 2 diabetes and/or insulin resistance greatly increases the chance that an individual will develop the metabolic syndrome.”
- Activity level (frequency of exercise).
- Smoking.
- Alcohol use.
- Age.
- Prescription medication use. Certain drugs that affect blood pressure, blood cholesterol, and blood sugar levels may contribute to metabolic disorder.
- Co-morbidities. The presence of metabolic disorder combined with either diabetes or heart-disease substantially increases your risk of serious complications.
Metabolic Syndrome and Gender
Due to hormonal differences and other distinguishing sex characteristics, women experience metabolic syndrome more often than men. Data gathered by the NIMS (National Institute of Medical Sciences) shows that approximately 29% of American women have the condition compared to 23% of American men.
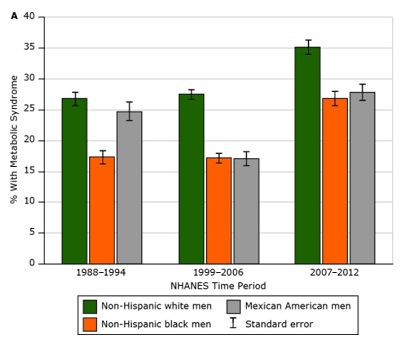
Metabolic Syndrome and Race
The data shows that generally speaking, non-Hispanic whites are at the highest risk of developing metabolic syndrome. This is true for both men and women. The chart below from the Centers for Disease Control (CDC) shows metabolic syndrome rates among men, broken up by race.
How Is Metabolic Syndrome Diagnosed?
 As outlined previously, metabolic syndrome is a “cluster” of conditions and not a condition itself.
As outlined previously, metabolic syndrome is a “cluster” of conditions and not a condition itself.
Metabolic syndrome is diagnosed when a patient experiences least three of five conditions simultaneously: clinical obesity (BMI of 30 or above), high fasting blood sugar (as seen in diabetic patients), elevated triglycerides, high blood pressure, and low levels of high-density lipoprotein (often abbreviated as “HDL,” the “healthy cholesterol”).
Therefore, to diagnose the presence of metabolic syndrome, a doctor must determine whether the patient fits the above criteria. Fasting blood sugar, triglyceride, and HDL cholesterol counts can all be assessed through blood tests, with results typically available within 24 hours. BMI is determined through a fast and easy standardized calculation using weight and height. Online BMI calculators can do the tabulation for you, or BMI analysis can be performed at any doctor’s office. Blood pressure, likewise, is generally measured at any routine visit to the doctor.
How Is Metabolic Syndrome Treated and Reversed?
Given the widespread prevalence of metabolic syndrome in the population, the natural question becomes how to treat – or even potentially reverse – metabolic syndrome before it leads to permanent damage. Here are the best-known interventions to combat metabolic syndrome:
- Switch to a whole-foods diet. Popular examples of these types of eating plans include Whole 30, Mediterranean Diet, Paleo Diet, and others.
- Limit sugar intake. Contrary to popular belief, sugar (especially added sugar in processed foods) is the primary dietary driver of obesity in the US population, not fat. This is because processed sugar is added to nearly every type of pre-packaged, processed food.
- Practice intermittent fasting (IF). Intermittent fasting is a proven method for improving metabolic health and restoring healthy metabolism.
- Get more exercise. Even moderate cardiovascular activity such as walking, practiced for at least 30 minutes a day, boosts metabolic function.
- Hormone replacement therapy (HRT). Hormone health is closely linked to metabolic health, particularly to the anabolic human growth hormone (HGH) and its partner hormone, insulin-like growth factor 1 (IGF-1). If you have an HGH or IGF-1 deficiency, replacement therapy can boost your levels and, in turn, your metabolic health.
The Connection Between Growth Hormone and Metabolic Syndrome
Human growth hormone is one of the primary anabolic (pro-growth) hormones in the human body. HGH is produced in the pituitary gland located in the brain.
One of the main roles of HGH and related IGF-1 is the promotion and regulation of healthy metabolism.
Throughout the day, but especially during sleep, the pituitary releases HGH in pulsatile secretions into the blood. Traveling through the blood, HGH arrives at the liver. There, it signals for the release of its “partner” hormone, insulin-like growth factor-1 (IGF-1). Together, HGH and IGF-1 promote healthy fat burning and energy use. These hormones are critical for stopping the development of the metabolic syndrome.
Because the optimal production and release of IGF-1 depends on circulating HGH levels, individuals with untreated HGH deficiencies (a condition known as growth hormone disorder or “GHD”) also develop an IGF-1 deficiency. As a result, a growth hormone deficiency increases the chances of emerging metabolic syndrome later on.
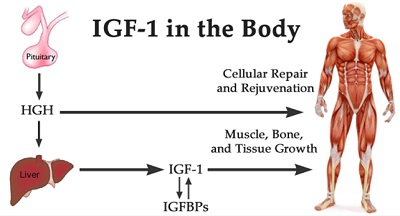
Research shows that proper blood levels and ratios between “IGF-1, GH, and insulin conform a finely regulated axis that inform cells about the nutritional status of the organism so that they can either undergo apoptosis/senescence/quiescence or, to the contrary, grow and differentiate.”
IGF-1 Binding Proteins and Metabolic Syndrome
Levels of IGF-1 binding proteins (IGFBP) — which transport IGF-1 and increase its half-life — are often compromised in individuals with obesity and/or metabolic syndrome: “Unregulated levels of IGFs/IGFBPs have been associated with the development of glucose intolerance and metabolic syndrome.”
The chart below shows lowered counts of both IGF-1 and its binding proteins (IGFBPs) in metabolic syndrome (MS) patients compared to a control group with a healthy metabolism.
The Bottom Line: How Can Metabolic Syndrome Be Prevented?
By following the lifestyle modifications (especially switching to a whole-foods, unprocessed low-sugar diet and increasing activity levels), you will equip your body with the tools it needs to maintain ideal metabolic health. Especially for aging Americans, declining hormone health — particularly as evidenced by falling growth hormone levels — can be a precipitating risk factor for metabolic syndrome.
If you suspect that you or a loved one have an undiagnosed growth hormone disorder or are experiencing the signs of metabolic syndrome discussed in this article, schedule an appointment with an experienced endocrinologist for a thorough evaluation of your hormone health. If necessary, maintaining your HGH levels (and, in turn, your IGF-1 levels) through hormone therapy can fortify your metabolic health for years to come.

