The health challenges that women experience during the phase of life known as menopause can be disorienting, disturbing, and, sometimes, even dangerous.
Here is everything you need to know about women’s hormones, menopause and its symptoms, how to protect your health while experiencing the condition, and even how to potentially delay its onset.
What Causes Menopause in Women?
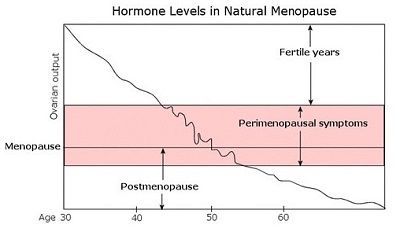
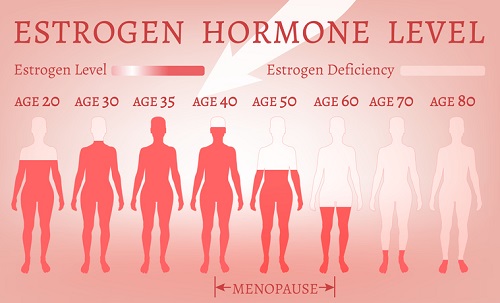
Menopause occurs as a cascade of physiological events that culminate in the end of a woman’s monthly menstrual cycle. The menstrual cycle is also popularly known as a “period.” The process begins when a woman’s ovaries stop producing as much estrogen – the most important female sex hormone – in the same amounts as they previously produced distributed the hormone earlier in life. The initial stage of the menopausal process is known as “perimenopause.”
Once estrogen levels drop consistently over a period of months or years, the ovaries no longer release an egg for fertilization and the period then stops.
Once a woman has not had her period for 12 months, she moves clinically into the stage known as menopause.
When Do Women Typically Begin to Experience the Symptoms of Menopause?
Menopause occurs around age 40-55 in most women. However, in some rare cases, women begin to see the symptomatic onset of menopause much younger – as early as their 20s. Therefore, it’s important to keep in mind that every woman’s journey is different. Nonetheless, the chart below offers a rough timeline for the process in most women.
An Important Note on Surgical Menopause
It’s important to note that, for a small subset of the female population, menopause begins following a medical procedure called a “bilateral oophorectomy,” during which both of the ovaries are removed. Oophorectomies are often preferred at the same time as hysterectomy, a more common removal of the uterus, or womb. For women receiving a bilateral oophorectomy, the symptoms of menopause will begin soon after the operation. This is called “surgical menopause.”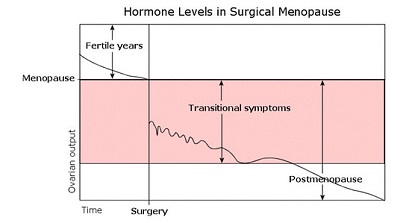
What Hormones Are Involved in Women’s Menopause?
The main driver of menopause in women is falling estrogen levels. Estrogen is the main sex hormone in the female physiology, meaning that it is primarily responsible for reproductive health.
Additional hormones impacted by menopause can include:
- Progesterone. As the other female sex hormone, progesterone is also produced in the ovaries. It plays a critical role in regulating the menstrual cycle and preparing the uterus for pregnancy. Progesterone levels decline significantly during menopause along with estrogen.
- Testosterone. Contrary to popular belief, testosterone is not just a male sex hormone. Women’s ovaries produce testosterone as well (although in much smaller quantities than in men), which plays a critical role in maintaining a healthy sexual libido. When the ovaries stop producing estrogen, they also cease testosterone production.
- Human growth hormone (HGH). The hormonal shifts seen in menopause affect the function of the hypothalamic-pituitary-adrenal axis (HPA axis), a network of glands and hormones that includes human growth hormone (HGH).
Menopausal women treated with supplemental estrogen via hormone replacement therapy (HRT) also benefit from elevated HGH levels compared to untreated menopausal women (more on the role of HGH in menopause later).
The 34 Signs and Symptoms of Menopause
The human body has estrogen receptors located throughout, so when levels drop significantly (as they do in menopause), the effects can be widespread – impacting every organ and its function. The graphic below illustrates all of the estrogen receptors in the body.
As promised, here are 34 of the most common signs and symptoms of menopause, broken down into five categories: initial symptoms occurring at the onset of menopause, mental symptoms, emotional symptoms, physical symptoms, and, finally, the most serious/most painful symptoms that some women experience.
The Initial Signs of Menopause (What to Expect at the Beginning)
- Hot flashes.
- Irregular period.
- Tender breasts.
- Low libido (loss of interest in sex).
- Vaginal dryness.
- Bladder issues (incontinence).
Mental Symptoms of Menopause
- Difficulty falling asleep.
- Impaired memory.
- Difficulty concentrating.
- Dizziness.
- Panic attacks.
Emotional Symptoms of Menopause
- Mood Swings.
- Anxiety.
- Depression.
- Loss of interest in daily activities.
- Irritability.
Physical Symptoms of Menopause
- Unwanted weight gain.
- Night sweats.
- Heart palpitations (skipping a beat).
- Bleeding gums.
- Dry skin.
- Hot flashes.
- Tingling hands and feet or “pins and needles” (paresthesia).
- Hair loss.
- Breast tenderness.
- Body odor.
- New allergies.
- Brittle nails.
- Gum disease.
The Most Painful/Most Severe Symptoms of Menopause
- Joint pain.
- Headaches.
- Osteoporosis (weakening of the bones).
- Digestive disorders.
- Muscle tension.
What Is the Role of Human Growth Hormone in Menopause?
Human growth hormone (HGH) is an important anabolic hormone, meaning that it promotes the healthy development and maintenance of various tissues throughout the body. HGH performs the following important tasks in the human body:
- Maintains ideal body composition (body fat distribution).
- Strengthens bones.
- Builds lean muscle.
- Promotes healthy metabolism (fat burning).
- Maintains high energy levels.
- May protect heart health.
The clinical data shows that HGH levels decline among women as they age, which “may lead to depression in growth and weight gain, changes in body composition, and metabolic impairment” – symptoms that are also seen in postmenopausal women. The chart below shows the declining levels of HGH and its partner hormone, insulin-like growth factor 1 (IGF-1) that occur across the lifespan.
The most interesting question for the provision of practical healthcare is how HGH levels are related to the occurrence or severity of menopause. Can HGH replacement therapy help treat the severity and/or duration of menopausal symptoms in women?
How Can HGH Replacement Therapy Help Menopausal Women Treat Their Symptoms?
Menopausal women may experience real therapeutic benefits from HGH therapy. Owing to the many health-promoting activities of HGH discussed earlier, the hormone may benefit women experiencing menopause in a number of ways explored below:
- Prevents the weakening of bones (osteoporosis). According to data from the National Osteoporosis Foundation, one in two women over 50, in fact, will break a bone due to osteoporosis as she moves into her golden years due to the hormonal shifts that occur during menopause, including declining HGH levels. One of the primary roles of HGH is to fortify bone strength.
- Maintains muscle mass. As we mentioned previously, muscle loss is one of the common symptoms of menopause. As an anabolic hormone, HGH protects muscle tissue, preventing its breakdown due to menopause or other causes.
- Stops unwanted weight gain. Fat accumulation, especially around the mid-section, is a common symptom of menopause. HGH helps keep your energy levels high and your fat metabolism in high gear.
- Relieves joint pain. Chronic joint pain, often due to arthritis, is a debilitating physical symptom of menopause. HGH replacement therapy, by tamping down inflammation and other underlying causes of arthritic pain, can provide much-needed relief from the pain commonly associated with menopause.
- Protects mental health. Studies have shown that, in women experiencing menopause and others with a diagnosed growth hormone disorder (GHD), replacement therapy improves markers of mental health. Several bodies of research into the connection between HGH and mental health conclude that HGH replacement therapy “improves psychological well-being and the quality of life” in patients with HGH deficiencies.
- Improved skin quality. Menopause often causes dry, itchy skin. HGH helps to keep skin supple, maintaining a brighter, more youthful appearance.
Can Menopause Be Delayed?
 One of the great areas of interest for doctors and institutions specializing in anti-aging medicine is how to delay or even potentially eliminate the occurrence of menopause. Although menopause is popularly accepted as a “natural” part of the aging process, there is not necessarily any biological law that dictates that it must occur.
One of the great areas of interest for doctors and institutions specializing in anti-aging medicine is how to delay or even potentially eliminate the occurrence of menopause. Although menopause is popularly accepted as a “natural” part of the aging process, there is not necessarily any biological law that dictates that it must occur.
The field of anti-aging research is rich with experimental models for delaying menopause by 20 years or more.
Innovative medical research and improving technology will likely result in even more promising advances in this important area of women’s healthcare.
In the meantime, if you are a woman beginning menopause, there are steps you can take to minimize the impact on your quality of life.
What Strategies Can Minimize the Impact of Menopause on Women’s Quality of Life?
If you are a woman entering middle age, here are several strategies that you can incorporate to make the hormonal transition into menopause smoother and less symptomatic:
- Eliminate processed, sugary foods from diet in favor of whole foods with a focus on phytoestrogen-rich culinary options.
- Supplement with calcium and vitamin D.
- Limit caffeine and alcohol intake.
- Perform at least 30 minutes of moderate physical activity each day.
- Estrogen replacement therapy.
- HGH replacement therapy.
If you are concerned about the impact that menopause is currently having (or may have in the future) on your quality of life, the time is now to start preparing. With the combined interventions above, you will put yourself in the best position to overcome the challenges of menopause and maintain the quality of life that you hope to keep as you move through the years.


